EMERGENCY HEALTH WORKFORCE POLICIES TO ADDRESS COVID-19Introduction
0 Comments
 Essential health care workers are putting their lives on the line as they treat and attempt to control the spread of COVID-19. This webinar examines the concept of Hazard Pay, defined by the U.S. Department of Labor as “additional pay for performing hazardous duties or physical hardship.” The panel provides a brief overview of current hazard pay proposals, examines the need and impact of hazard pay for low and high wage essential health care workers, and offers an economist perspective and possible approaches.  This Webinar examines the implications of COVID-19 for the oral health workforce. Speakers address the impact of COVID-19 on dental practices, share innovations - including teledentistry and integrated oral health, primary care, and public health - and discuss implications and policy needs for future practice to ensure oral health care access.
MD, MPH, of the Association of State and Territorial Health Officials (ASTHO) talks about the tool’s potential to bring greater awareness of contact tracing to its members with realistic measures of staff volume and mixed workforce, as well as coordination considerations when expanding staffing resources. Chris Aldridge, MSW, at the National Association of County and City Health Officials (NACCHO) discusses the importance of being able to change the tool parameters to see local level needs to help health departments project current and future caseloads. relevant resources
 Moderated by Lynn Goldman, Dean of the George Washington University Milken Institute School of Public Health, this session highlights the importance of public health’s role in building stronger communities and considerations for scaling-up contact tracing. Jeffrey Levi, PhD, of the George Washington University Milken Institute School of Public Health provides a national historical overview of public health workforce spending decline and the potential investments needed to rebuild the public health infrastructure. Amanda D. Castel, MD, MPH, of the George Washington University Milken Institute School of Public Health shares her observations as a volunteer of the DC Health Department, providing an in-depth look into the on-the-ground work by public health workers and the implications of COVID-19 response on other preventative health services. Alan E. Greenberg, MD, MPH, of the George Washington University Milken Institute School of Public Health and School of Medicine and Health Sciences describes past experiences from the HIV/AIDS epidemic that may help inform the pandemic response. relevant resources
 Lawrence Deyton, MSPH, MD, of the George Washington University School of Medicine and Health Sciences discusses the clinical public health curriculum work at GW and how these principles are being deployed in response to COVID-19. David Edelman, MD, of Columbia University Vagelos College of Physicians and Surgeons provides a student’s perspective, noting especially how interprofessional students can build on existing structures and relationships to mobilize in a crisis. Veronica Thierry Mallett, MD, MMM, of Meharry Medical College shares community strategies and approaches Meharry has undertaken to improve health equity during the pandemic and future recommendations for health care providers and policy makers. relevant resources
 Dr. Michael Fraser, Chief Executive Officer of the Association of State and Territorial Health Officials (ASTHO) provides an overview of the need for contact tracing in the COVID-19 pandemic and discusses the opportunity to build the capacity of the future public health workforce. Dr. Nilesh Kalyanaraman, Health Officer of the Anne Arundel County Department of Health, outlines the county level approach to contact tracing in Anne Arundel County and presents unique challenges and opportunities of the experience to date. relevant resources
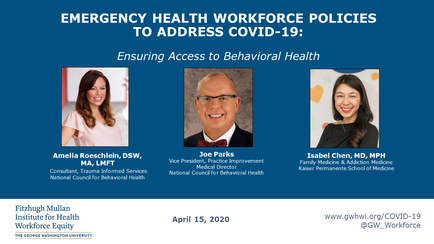 Joe Parks, M.D, Medical Director, National Council for Behavioral Health discusses federal and state policies that enable ongoing access to behavioral health during the COVID19 crisis. and outlines additional policies that are needed to further support patients and providers during the pandemic. Amelia Roeschlein, DSW, MA, LMFT, and Consultant, Trauma Informed Services discusses resilience techniques and how to support health care providers during the pandemic. The session concludes with a discussion on how we can prepare for a likely surge in behavioral health needs in the coming months. READ SUMMARY relevant resources
Resources
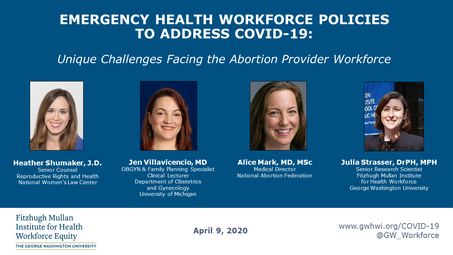 Alice Mark, Medical Director for the National Abortion Federation, discusses underlying challenges facing abortion providers and how these have been exacerbated by the COVID19 crisis. Heather Shumaker, Senior Counsel for Reproductive Rights and Health at the National Women’s Law Center, explains current state policies and litigation affecting the abortion provider workforce. Jen Villavicencio, OB/GYN and Clinical Lecturer at the University of Michigan, talks about the impact of abortion care policies in Michigan and changes that providers are making to reduce risks of exposure. 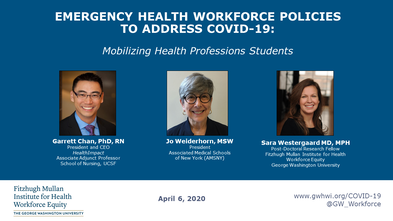 Jo Wiederhorn, MSW, of the Associated Medical Schools of New York (AMSNY) discusses the early graduation of fourth year medical students in New York State and the proposed roles these new physicians would have in the COVID-19 response. Garrett Chan, PhD, RN, of HealthImpact outlines potential strategies for nursing students in California to aid in the pandemic while also maintaining academic and practice partnerships. READ SUMMARY relevant resources
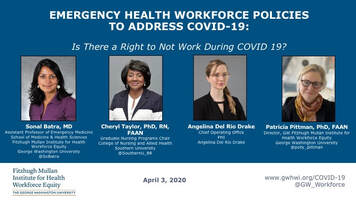 This session builds on a prior webinar entitled Why Occupational Standards Matter and focuses on the question of whether health personnel have the right NOT to work when they feel their health or their family’s health, or life, is in danger. The WHO affirms that employers must "allow workers to exercise the right to remove themselves from a work situation that they have reasonable justification to believe presents an imminent and serious danger to their life or health ..." without undue consequences. Panelists from three professions - medicine, nursing and home care - discuss the different ways in which they are experiencing tensions between the social mission of their work, on the one hand, and its limits when employers have not provided adequate worker protection, on the other. They also discuss policies and practices that would help alleviate this tension, including child care, housing, and hazard pay. READ SUMMARY relevant resources
relevant resources
 This session asks whether national enforceable occupational standards matter, and if so, why the United States has no occupational safety standards for airborne pathogens. The World Health Organization has issued guidance with a list of 13 health worker rights relevant to the COVD-19 pandemics, 8 of which refer to either the right to obtain training in infection control, or the right to appropriate protective gear. Panelists discuss why issuing a national safety standard is so important to ensuring those rights in the current situation. They also explore why employers and the Trump administration have opposed issuing an emergency standard. READ SUMMARY relevant resources
 This session focuses on emergency measures states can take to remove certain restrictions on the scope of practice of a variety of health professions, as a strategy to maximize the current workforce capacity. The COVID-19 crisis makes the basic principle of having all personnel working at the top of their education and license especially urgent, both as a way to enhance efficiency and to reduce frustration among health care team members. Panelists review changes that should be considered and then discuss executive orders already issued by governors in ten states. READ SUMMARY
relevant resources
Policy: Center for Connected Health Policy Federation of State Medical Boards Practice: American Academy of Family Physicians CMS
|
Webinar Introduction
Categories
All
|
© 2024 | 2175 K Street NW, Suite 250, Washington, DC 20037 | (202) 994-3423 | GW Privacy Policy